When you receive medical treatment, your authorization matters. Express consent and implied consent represent two distinct ways patients grant permission for medical care, and the differences between them carry significant legal weight under Florida law. Understanding these distinctions helps patients recognize when their consent rights may have been violated and whether they have grounds for a medical malpractice claim.
Florida’s informed consent framework, codified in Fla. Stat. § 766.103, establishes specific requirements for how healthcare providers must obtain patient authorization. When providers fail to meet these requirements, injured patients may pursue legal action. The type of consent involved—express or implied—affects both the nature of the claim and what must be proven.
What Is Express Consent in Medical Treatment?
Express consent occurs when a patient actively and clearly communicates agreement to a proposed treatment or procedure. This represents the most direct form of patient authorization and provides the strongest legal foundation for medical care.
How Providers Obtain Express Consent
Healthcare providers typically obtain express consent through a formal process that documents the patient’s agreement. For surgical procedures, invasive treatments, and high-risk interventions, this almost always involves written consent forms that the patient signs after receiving information about the proposed care.
Verbal express consent also qualifies as valid authorization. A patient who verbally agrees to a procedure after a physician explains it has provided express consent. However, written documentation creates clearer evidence of what was communicated and agreed upon.
The express consent process requires a two-way exchange. The provider must offer information, and the patient must actively signal agreement. Silence or passive acceptance does not constitute express consent.
What Information Must Be Disclosed
Under Florida law, express consent must be truly informed to be valid. Fla. Stat. § 766.103(3)(a) requires that a reasonable individual receiving the disclosure would have a general understanding of essential information about the proposed treatment.
Florida requires providers to disclose the following elements when obtaining express consent:
- The nature of the proposed procedure or treatment and its intended purpose
- The substantial risks and potential complications inherent in the treatment
- Medically acceptable alternative treatments that exist for the condition
- The risks and benefits associated with those alternatives
- The likely consequences of refusing the proposed treatment
The extent of required disclosure depends on the circumstances of each case. More complex or risky procedures demand more extensive explanation. According to Thomas v. Berrios, 348 So. 2d 905 (Fla. 2d DCA 1977), expert testimony typically establishes what disclosure a reasonable medical practitioner would provide in similar circumstances.
The Legal Strength of Express Consent
Express consent, particularly when documented in writing, creates significant legal protection for healthcare providers. Under Fla. Stat. § 766.103(4), a written consent form that meets statutory requirements raises a rebuttable presumption that the consent was valid.
This presumption means that if a provider can produce a properly executed consent form, the burden shifts to the patient to demonstrate that the consent was somehow deficient. The patient might prove this by showing that oral representations contradicted the written form or that material information was withheld despite what the form stated.
The Florida Supreme Court addressed this dynamic in Public Health Trust of Dade County v. Valcin, 507 So. 2d 596 (Fla. 1987), establishing that fraudulent oral misrepresentations can vitiate an otherwise valid written consent form. This case confirms that written consent creates a presumption, not an absolute bar to claims.
What Is Implied Consent in Medical Treatment?
Call us today at (305) 694-2676 or
contact us online for a free case evaluation.
Hablamos español.


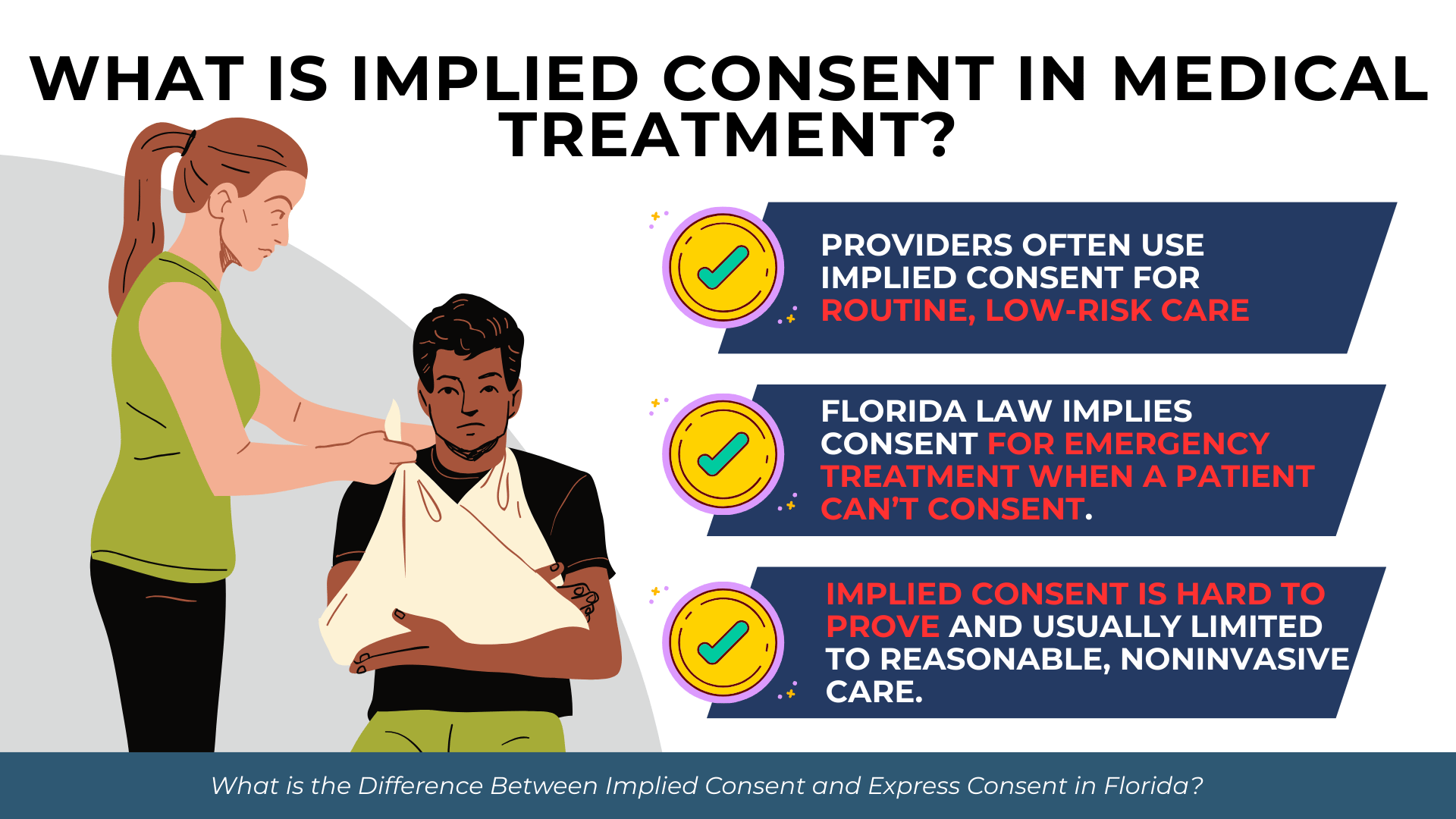
Implied consent arises from a patient’s conduct or circumstances rather than explicit verbal or written agreement. The patient’s actions suggest willingness to receive treatment without stating it directly.
When Implied Consent Applies
Healthcare providers commonly rely on implied consent for routine, low-risk medical care where formal consent processes would be impractical. The law recognizes implied consent in several circumstances.
Implied consent typically applies in the following situations:
- A patient extends their arm for a blood draw or injection without verbal confirmation
- A patient arrives for a scheduled routine appointment and cooperates with standard examination procedures
- A patient presents themselves at a medical facility seeking care for an obvious condition
- A patient follows instructions during a physical examination without objection
- A patient’s continued presence and cooperation during treatment suggests agreement
The key principle underlying implied consent is that the patient’s behavior would lead a reasonable person to conclude that authorization exists. Rolling up a sleeve when a nurse prepares to draw blood implies consent to that blood draw, even without spoken words.
The Emergency Exception to Consent Requirements
Florida law recognizes an important form of implied consent in emergency situations. When immediate medical intervention is necessary to preserve life or prevent serious harm, and the patient cannot provide consent, the law presumes the patient would want life-saving treatment.
This emergency exception applies when a patient is unconscious, incapacitated, or otherwise unable to communicate. The provider must reasonably believe that treatment is immediately necessary and that delay to obtain consent would endanger the patient.
The emergency exception reflects a policy judgment that most people would choose necessary medical care over death or serious injury. However, this implied consent extends only to treatment necessary to address the emergency. Once the patient is stabilized or regains capacity to consent, providers must return to standard consent procedures.
Limitations of Implied Consent
Implied consent has significant limitations that affect its legal reliability. Because it lacks explicit documentation, proving that implied consent existed can become challenging if a dispute arises.
Implied consent generally does not extend to invasive procedures, surgical interventions, or treatments carrying substantial risk. A patient presenting to an emergency room with a broken arm implicitly consents to examination and basic treatment, but not necessarily to surgery. More significant interventions require express consent.
The scope of implied consent is also limited to what a reasonable patient would expect under the circumstances. A patient who consents to a diagnostic procedure has not implicitly consented to treatment based on the diagnosis. Each distinct intervention requires its own authorization.
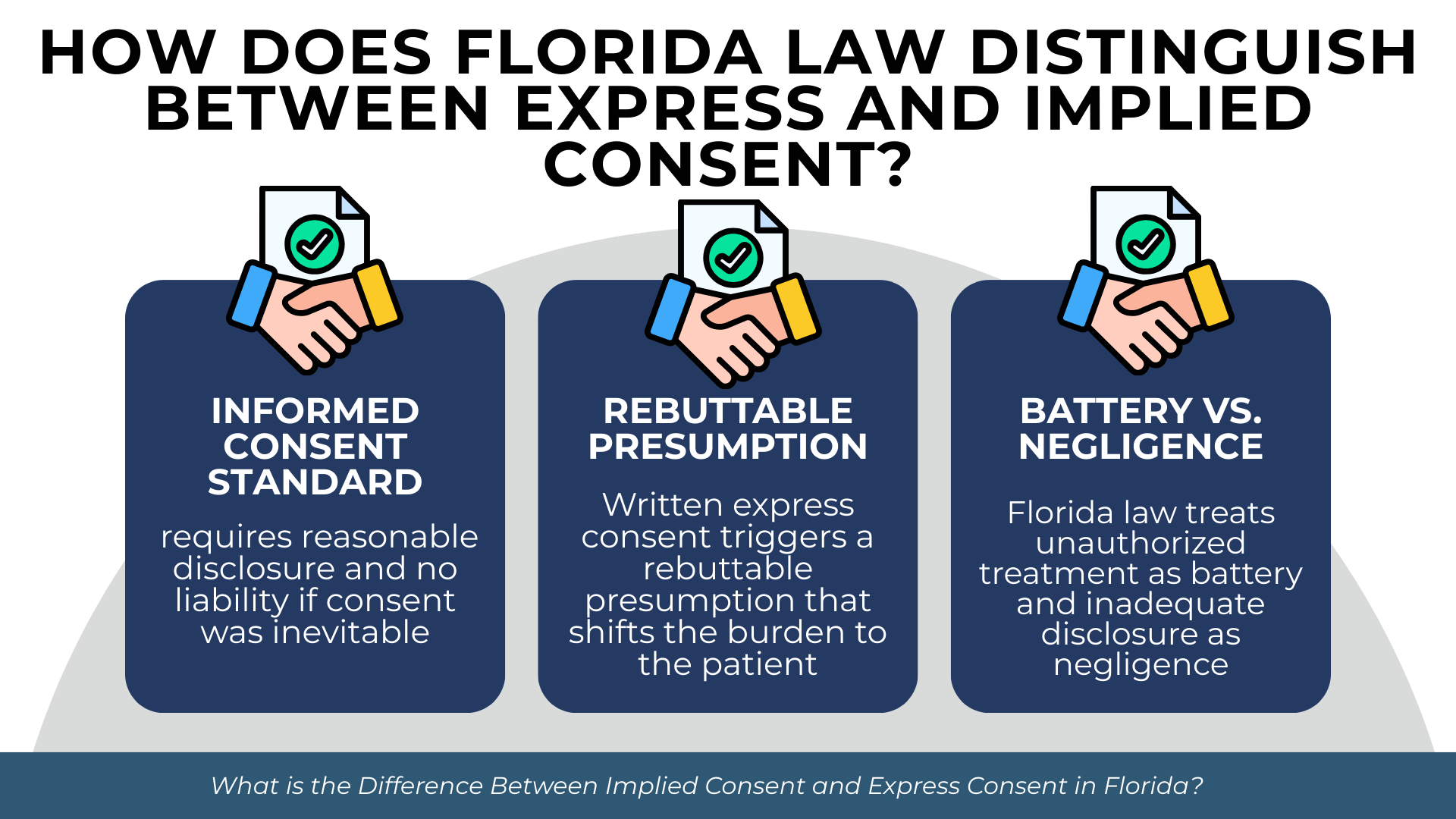
How Does Florida Law Distinguish Between Express and Implied Consent?
Florida’s statutory framework addresses consent primarily through the lens of informed consent requirements. The distinction between express and implied consent becomes legally significant when evaluating whether a provider met applicable standards and what type of claim a patient may pursue.
Florida’s Informed Consent Standard Under § 766.103
Florida employs a hybrid standard for informed consent that combines physician-centered and patient-centered elements. Under Fla. Stat. § 766.103(3)(a), no recovery is allowed when a provider obtained consent in accordance with the accepted standard of medical practice among similar providers, and a reasonable individual would have understood the procedure, alternatives, and substantial risks.
This standard requires both professional reasonableness and patient comprehension. The provider must follow what similar practitioners would do, and the disclosure must enable a reasonable person to understand the essential information.
Florida also recognizes an objective causation defense under Fla. Stat. § 766.103(3)(b). Even if disclosure was inadequate, no recovery is permitted if the patient would reasonably have undergone the treatment anyway had proper information been provided. This acknowledges that some disclosure failures do not actually change patient decisions.
The Rebuttable Presumption of Written Consent
Written express consent triggers the rebuttable presumption established in Fla. Stat. § 766.103(4). This creates a meaningful difference from implied consent, which carries no such presumption.
When a provider relies solely on implied consent, no presumption of validity exists. The provider must demonstrate through other evidence that the patient understood and agreed to the treatment. In contrast, a written consent form shifts the initial burden to the patient.
However, as Valcin established, the presumption is rebuttable. Evidence that providers made fraudulent misrepresentations, withheld material information, or obtained signatures under circumstances that precluded genuine understanding can overcome the presumption.
Battery Versus Negligence Claims
The type of consent involved—and the nature of any violation—determines whether a patient’s claim sounds in battery or negligence. This distinction carries practical consequences for what must be proven.
Florida courts distinguish consent-based claims according to these principles:
- Battery claims arise when no consent was obtained at all, or when a fundamentally different procedure was performed than what was authorized
- Negligence claims arise when consent was obtained but the disclosure was inadequate to make the consent truly informed
- Battery claims do not require expert testimony because the lack of consent is itself the wrong
- Negligence claims require expert testimony to establish what a reasonable provider would have disclosed
- Battery claims may support punitive damages in egregious cases
- Negligence claims typically involve compensatory damages only
According to Gouveia v. Phillips, 823 So. 2d 215 (Fla. 4th DCA 2002), the distinction turns on whether any meaningful consent existed. Performing a procedure without any authorization is battery. Performing a procedure with authorization but without adequate disclosure is negligence.
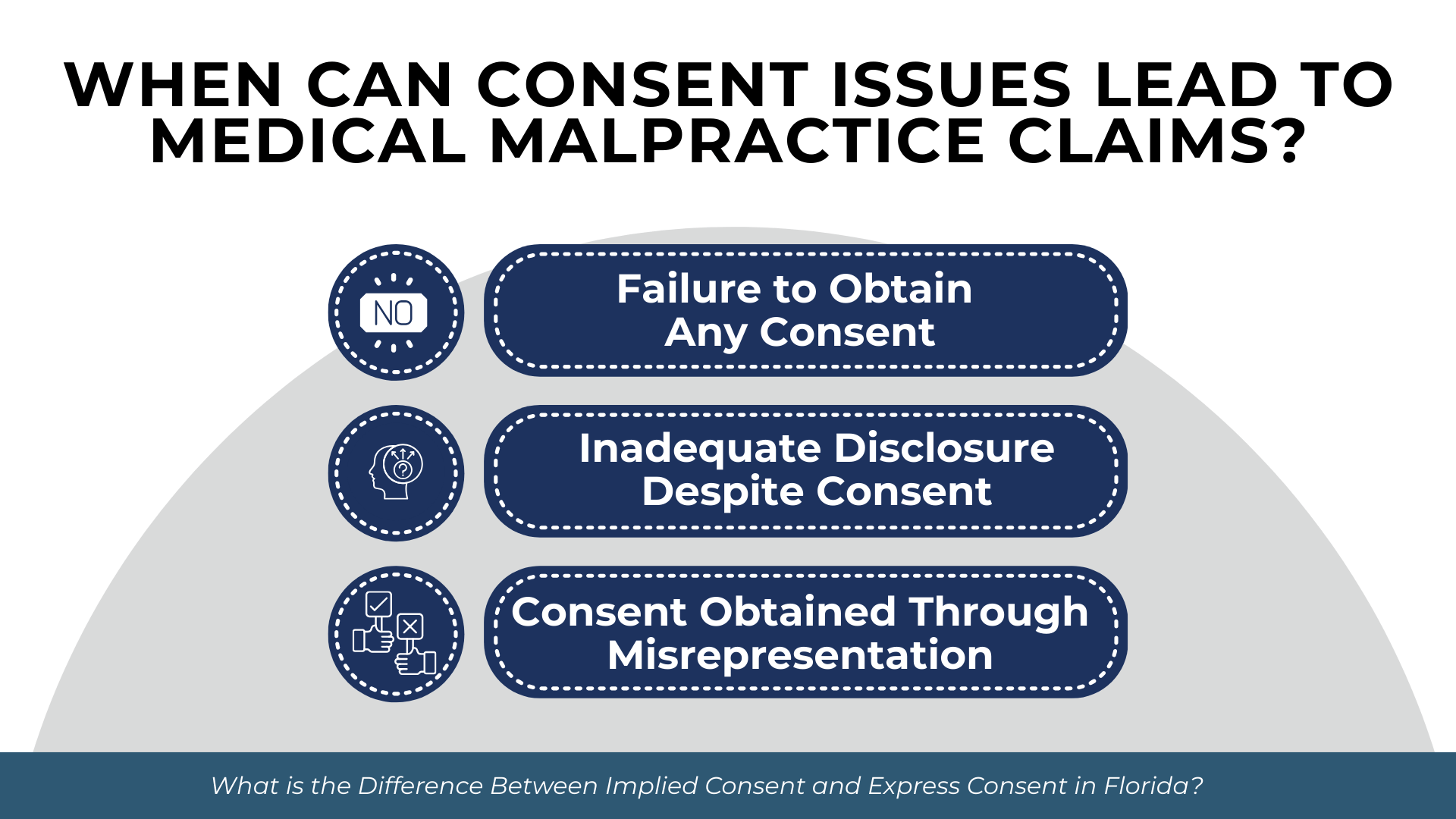
When Can Consent Issues Lead to Medical Malpractice Claims?
Consent violations can give rise to actionable claims under several theories. The viability of a claim depends on what occurred, what harm resulted, and whether the consent failure can be connected to that harm.
Failure to Obtain Any Consent
When a provider performs a procedure without obtaining any consent—express or implied—the patient may have a battery claim. Battery in the medical context means unauthorized touching, regardless of whether the treatment itself was performed competently.
This theory applies when providers proceed without asking, when patients expressly refuse treatment that is then performed anyway, or when providers perform substantially different procedures than those authorized. A patient who consents to surgery on the left knee but undergoes surgery on the right knee has not consented to the procedure actually performed.
Battery claims do not require proof that the treatment itself was negligent. The violation is the unauthorized touching, not the quality of care. However, plaintiffs still must prove that they suffered damages from the unauthorized procedure.
Inadequate Disclosure Despite Consent
More commonly, patients pursue negligence claims alleging that while consent was obtained, the disclosure was insufficient to make that consent meaningful. These claims assert that had adequate information been provided, the patient would not have agreed to the treatment.
Proving inadequate disclosure requires establishing what a reasonably prudent similar provider would have communicated under the circumstances. According to Ditlow v. Kaplan, 181 So. 2d 226 (Fla. 3d DCA 1965), Florida applies a professional standard asking what a reasonable medical practitioner in the community would disclose.
The plaintiff must also demonstrate that the inadequate disclosure caused harm. If the patient would have undergone the treatment regardless of additional information, or if the harm that occurred was unrelated to the undisclosed risks, the disclosure failure may not support recovery.
Consent Obtained Through Misrepresentation
When providers obtain consent through fraudulent misrepresentation of material facts, patients may challenge that consent even if a written form exists. Valcin established that oral misrepresentations can vitiate written consent.
This theory applies when providers affirmatively misstate risks, conceal known complications, or provide false information about alternatives. The misrepresentation must concern a material fact that would have affected the patient’s decision.
Proving fraudulent misrepresentation requires showing that the provider knew the information was false or acted with reckless disregard for its truth. This is a higher burden than ordinary negligence and may support additional remedies.
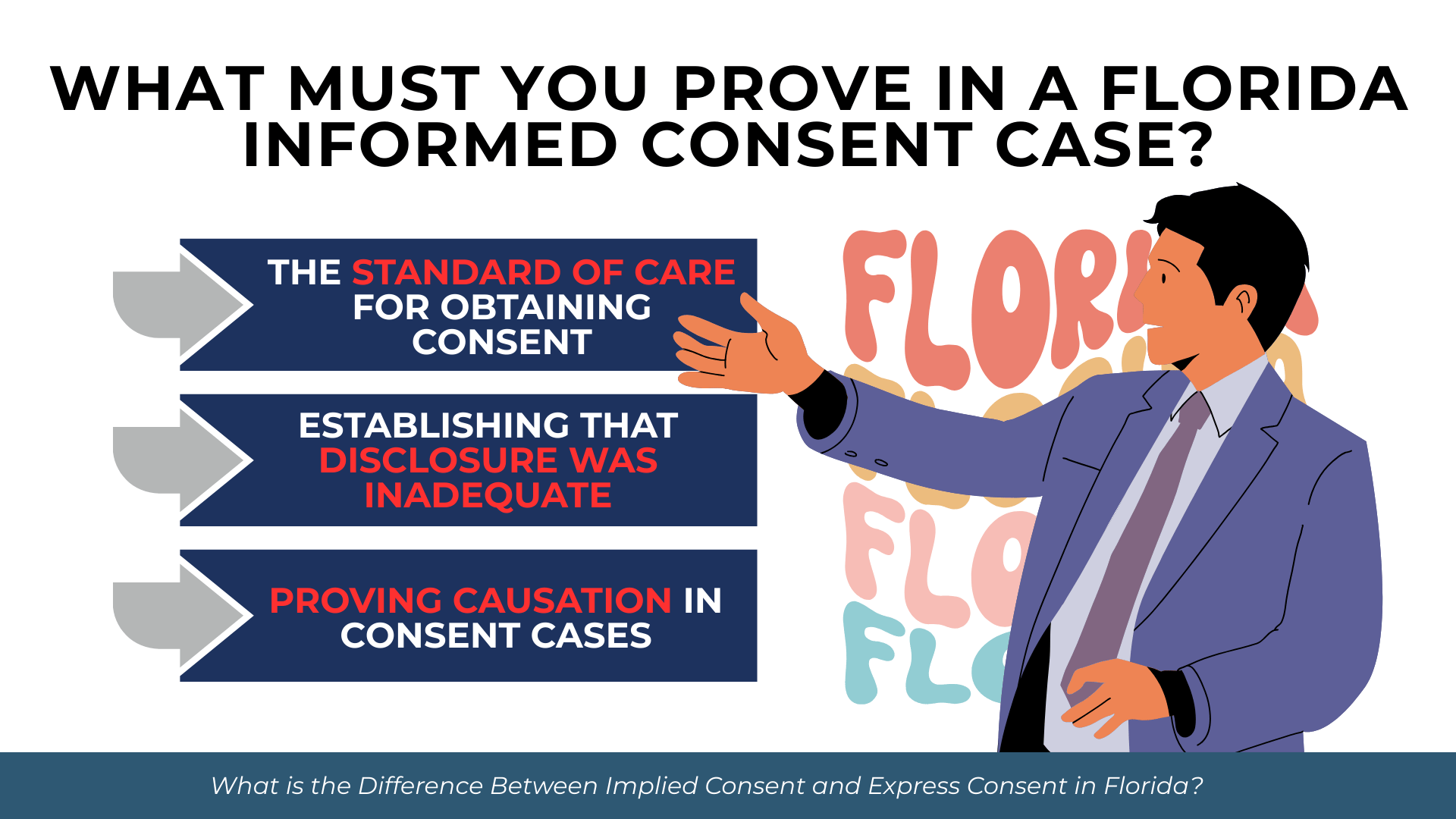
What Must You Prove in a Florida Informed Consent Case?
Get started with your complimentary case evaluation today;
call us at (305) 694-2676 or reach us online using our
secure contact form.


Succeeding on an informed consent claim requires proving specific elements under Florida law. The burden of proof falls on the plaintiff to establish each element by the greater weight of the evidence.
The Standard of Care for Obtaining Consent
Florida treats inadequate disclosure as a form of medical negligence governed by the same general framework as other malpractice claims. Under Fla. Stat. § 766.102, plaintiffs must establish the prevailing professional standard of care and show that the defendant’s conduct fell below that standard.
For consent claims, this means proving what information a reasonably prudent similar provider would have disclosed before the treatment in question. Expert testimony typically establishes this standard, though some disclosures may be so obviously necessary that lay understanding suffices.
The standard is not perfection. Providers need not disclose every conceivable risk. The question is whether the disclosure enabled a reasonable patient to understand the procedure, its substantial risks, and available alternatives.
Establishing That Disclosure Was Inadequate
Plaintiffs must prove that the provider’s actual disclosure fell short of what the standard required. This involves comparing what was communicated against what should have been communicated.
Evidence of inadequate disclosure may include the consent form itself, medical records documenting the consent conversation, testimony from the patient about what was said, and expert testimony about what information was missing. If material risks that actually occurred were not disclosed, this supports a finding of inadequacy.
Defendants often counter by pointing to written forms, arguing that the form demonstrates adequate disclosure. Plaintiffs may rebut this presumption by showing that oral communications contradicted or omitted information from the form.
Proving Causation in Consent Cases
Florida requires plaintiffs to prove that adequate disclosure would have led to a different decision. Under the objective standard in Fla. Stat. § 766.103(3)(b), the question is whether a reasonable patient in the plaintiff’s position would have declined the treatment if properly informed.
This causation element distinguishes consent claims from ordinary negligence. Even if disclosure was inadequate, no recovery is available if the patient would have proceeded anyway. This protects providers from liability when disclosure failures did not actually affect patient choices.
Additionally, plaintiffs must connect the consent failure to their injuries. If the harm resulted from risks that were properly disclosed, or from causes unrelated to the procedure, the inadequate disclosure may not have caused the damages claimed.
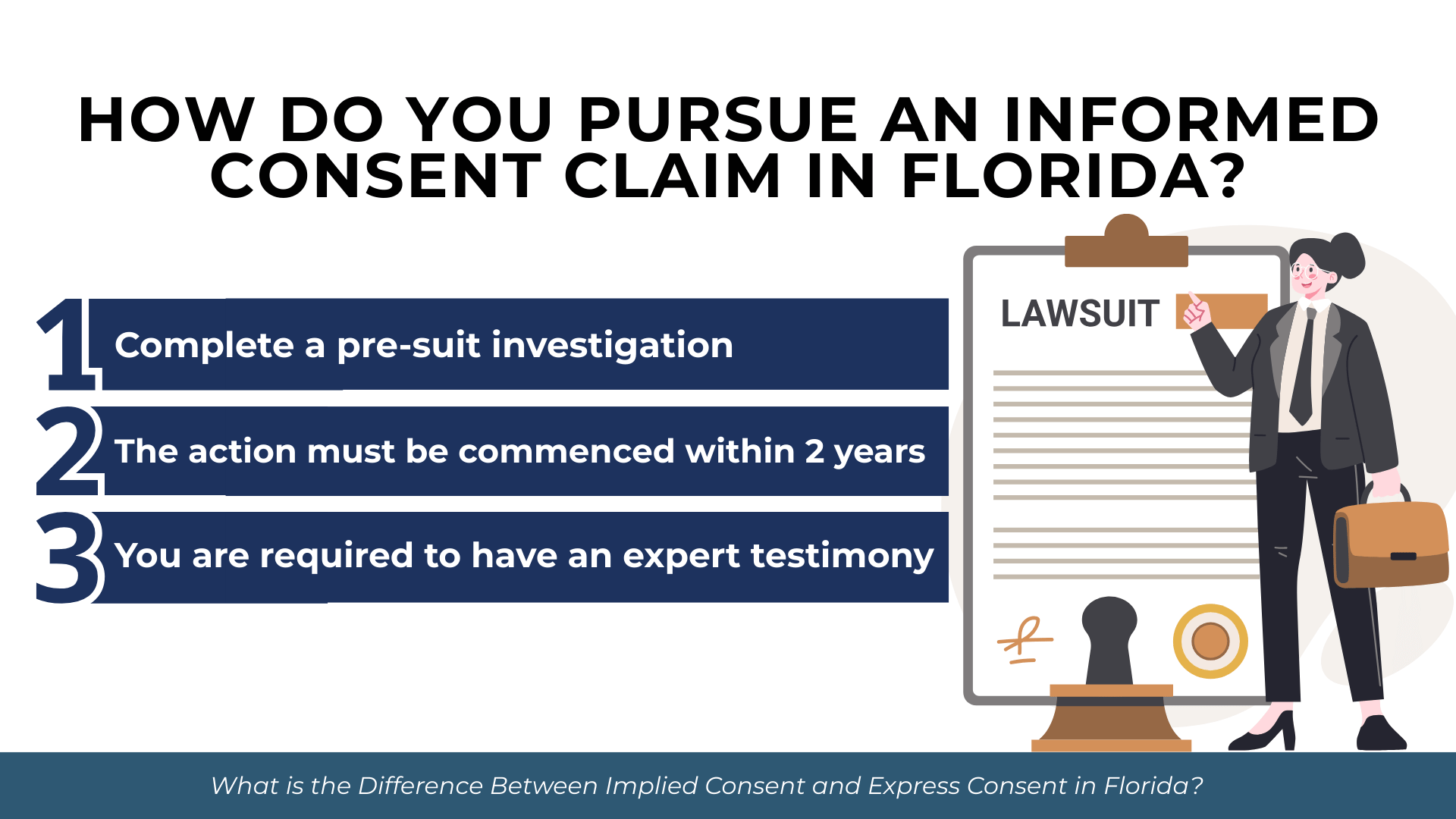
How Do You Pursue an Informed Consent Claim in Florida?
Florida imposes specific procedural requirements on medical malpractice claims, including those based on consent violations. Meeting these requirements is mandatory before filing suit.
Pre-Suit Investigation Requirements
Florida law requires plaintiffs to complete a pre-suit investigation before filing a medical malpractice complaint. Under Fla. Stat. § 766.203, this investigation must establish reasonable grounds to believe the defendant was negligent and that such negligence caused injury.
Before filing suit, plaintiffs must complete the following steps:
- Conduct a pre-suit investigation to determine that reasonable grounds exist to support the claim
- Obtain a verified written medical expert opinion corroborating the grounds for the claim
- Serve written notice of intent to initiate litigation on each prospective defendant by certified mail
- Include copies of all medical records relied upon by the expert with the notice
- Wait at least 90 days after serving notice before filing suit
The 90-day pre-suit period tolls the statute of limitations, meaning the time spent in pre-suit investigation does not count against filing deadlines. According to Hankey v. Yarian, 755 So. 2d 93 (Fla. 2000), this ensures claimants retain the full benefit of their original statutory time period.
Statute of Limitations for Consent Claims
Informed consent claims are subject to the same limitations periods as other medical malpractice claims. Under Fla. Stat. § 95.11(5)(c), the action must be commenced within 2 years from when the incident occurred or within 2 years from when it was discovered or should have been discovered with due diligence.
Florida imposes a 4-year statute of repose that bars claims filed more than 4 years from the date of the incident, regardless of when discovery occurred. This outer limit applies even if the patient could not reasonably have discovered the consent violation sooner.
Under Tanner v. Hartog, 618 So. 2d 177 (Fla. 1993), the limitations period begins when the patient has knowledge of the injury and a reasonable possibility that it was caused by medical malpractice. For consent claims, this may mean the period starts when the patient learns that material information was withheld.
Expert Testimony Requirements
Consent claims alleging negligent disclosure require expert testimony under Fla. Stat. § 766.102. The expert must establish what a reasonably prudent similar provider would have disclosed and opine that the defendant’s disclosure fell below that standard.
Experts must meet specific qualifications. Under Fla. Stat. § 766.102(5)(a), an expert testifying against a specialist must specialize in the same specialty and have devoted professional time during the 3 years immediately preceding the incident to active clinical practice, instruction, or research in that specialty.
Battery claims based on complete absence of consent may not require expert testimony because the lack of authorization is itself the wrong. However, most consent-based claims involve allegedly inadequate disclosure, which does require expert support.
Frequently Asked Questions About Medical Consent in Florida
Can a hospital perform surgery without my consent?
Generally, no. Surgery requires express consent except in genuine emergencies where you cannot provide consent and delay would endanger your life. Even in emergencies, the implied consent extends only to treatment necessary to address the immediate threat. Once you are stabilized or capable of consenting, providers must obtain your authorization before proceeding with additional treatment.
Does signing a consent form prevent me from suing for malpractice?
No. A signed consent form creates a rebuttable presumption that consent was valid, but you can challenge that presumption. Under Valcin, fraudulent oral misrepresentations can overcome a written consent form. You may also pursue claims if the written form itself failed to disclose material risks, or if the procedure performed differed substantially from what you authorized.
What if I was unconscious when treatment was provided?
Florida law recognizes implied consent for emergency treatment when you cannot provide authorization and immediate care is necessary to preserve life or prevent serious harm. Providers may treat you under these circumstances without express consent. However, this emergency exception is limited to genuinely necessary interventions. Treatment that can safely wait until you regain consciousness requires your actual consent.
How long do I have to file a claim for lack of informed consent in Florida?
You must file within 2 years of discovering the consent violation or within 2 years of when you should have discovered it with reasonable diligence. Florida also imposes a 4-year statute of repose that bars claims filed more than 4 years after the incident, even if you could not have discovered the violation sooner. The 90-day pre-suit period tolls these deadlines, so time spent in mandatory pre-suit investigation does not count against your limitations period.
Do I need an expert witness for an informed consent case?
For most consent claims alleging inadequate disclosure, yes. Expert testimony establishes what a reasonably prudent provider would have disclosed and whether the defendant’s disclosure fell short. The exception is battery claims based on complete absence of consent, where the lack of authorization itself is the violation. However, even battery claims require proof of damages, and expert testimony may be needed to establish the nature and extent of your injuries.
Protecting Your Rights When Consent Is Violated
The distinction between express consent and implied consent affects both how medical care should be authorized and what legal options exist when consent requirements are violated. Express consent, particularly in writing, creates documented evidence of patient authorization and provider disclosure. Implied consent serves practical purposes for routine care and emergencies but provides less legal protection for both parties.
Florida law requires that consent be truly informed, meaning patients must receive and understand material information about proposed treatments. When providers fail to meet disclosure requirements, or when they proceed without any consent at all, injured patients may have grounds for legal action.
If you believe your consent rights were violated during medical treatment, contact Prosper Injury Attorneys to discuss your situation.