When a radiologist fails to identify a tumor, misreads a fracture, or overlooks signs of a stroke on medical imaging, the consequences can be devastating. Patients may lose valuable treatment time, face disease progression, or suffer outcomes that could have been prevented with accurate interpretation. Florida law allows patients to pursue medical malpractice claims against radiologists whose diagnostic errors cause harm, but these cases require meeting specific legal standards and procedural requirements.
Radiology errors contribute significantly to the broader problem of diagnostic failure in American healthcare. According to BMJ Quality & Safety (2024), approximately 795,000 Americans die or become permanently disabled from diagnostic error annually. Radiologists play a central role in diagnosis across virtually every medical specialty, making their accuracy critical to patient outcomes.
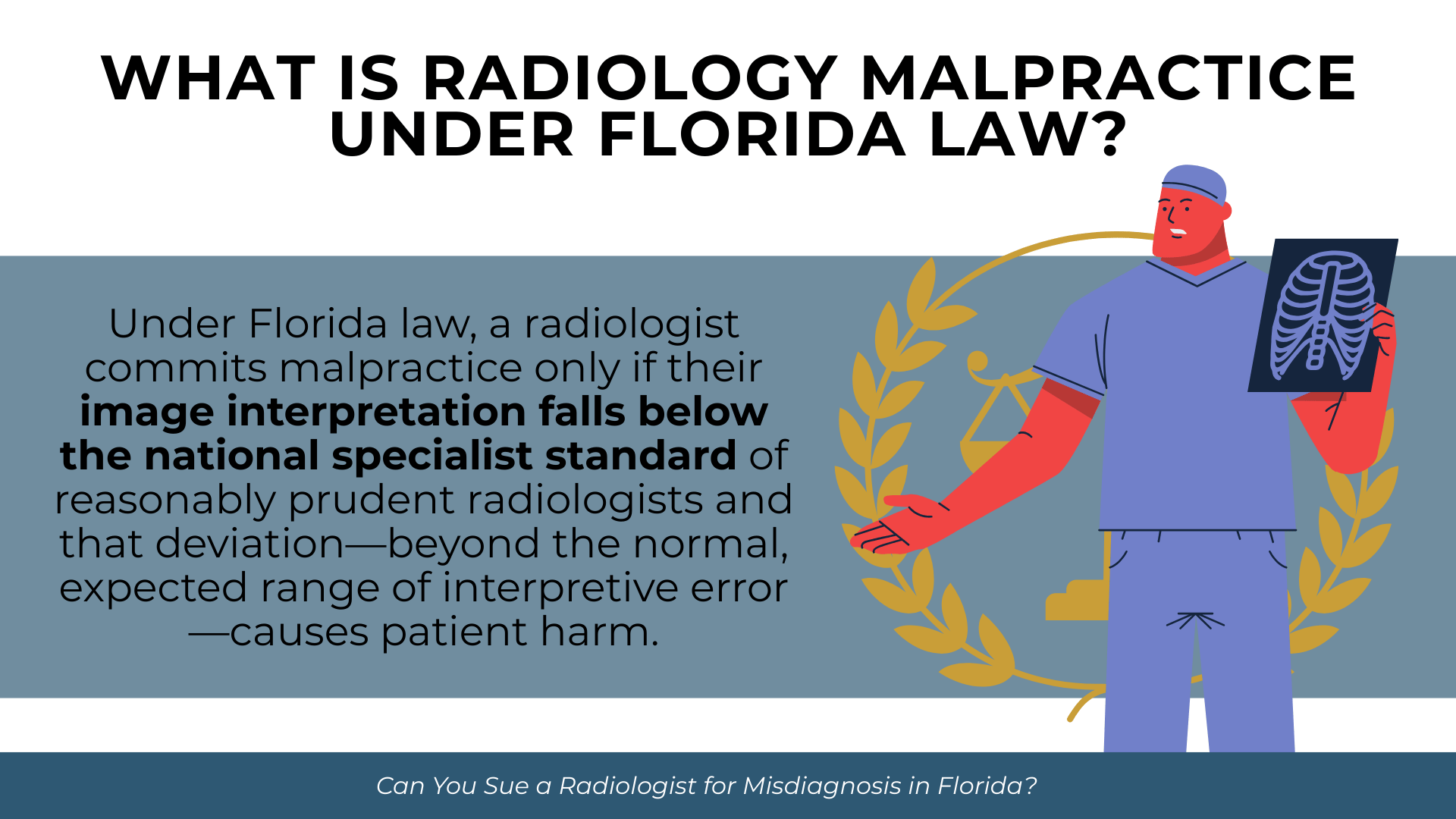
What Is Radiology Malpractice Under Florida Law?
Defining the Radiologist’s Standard of Care
Florida law defines the prevailing professional standard of care as “that level of care, skill, and treatment which, in light of all relevant surrounding circumstances, is recognized as acceptable and appropriate by reasonably prudent similar health care providers.” Under Fla. Stat. § 766.102, radiologists are held to a specialist standard when practicing within their specialty.
This means a radiologist’s image interpretation is measured against what other qualified radiologists would recognize as acceptable practice. Florida has largely moved away from a strict locality rule, applying a national professional standard for clinical care. A radiologist in Miami is expected to meet the same interpretive standards as one in Chicago or Los Angeles.
How Florida Courts Evaluate Radiology Errors
Radiology interpretation is inherently probabilistic rather than absolute. Not every missed finding constitutes malpractice. Courts evaluate whether the radiologist’s reading fell below what reasonably prudent radiologists would consider acceptable under the circumstances.
According to research published in the American Journal of Roentgenology (2014) and Insights into Imaging (2017), day-to-day radiology error rates range from 3-5%, while retrospective review reveals discrepancy rates of approximately 20-30%. These figures reflect the inherent difficulty of image interpretation rather than widespread negligence. The legal question is whether a specific error represents a deviation from acceptable practice or falls within the range of reasonable professional judgment.
The Difference Between Error and Malpractice
A radiology error does not automatically equal malpractice. Fla. Stat. § 766.102(3)(b) explicitly states that medical injury alone does not create an inference of negligence. To establish malpractice, the patient must prove the radiologist’s interpretation fell below the standard that reasonably prudent radiologists would meet and that this substandard care caused harm.
Some findings are subtle and reasonably missed even by competent radiologists. Others are so obvious that missing them represents a clear departure from acceptable practice. Expert testimony typically determines which category applies in a given case.
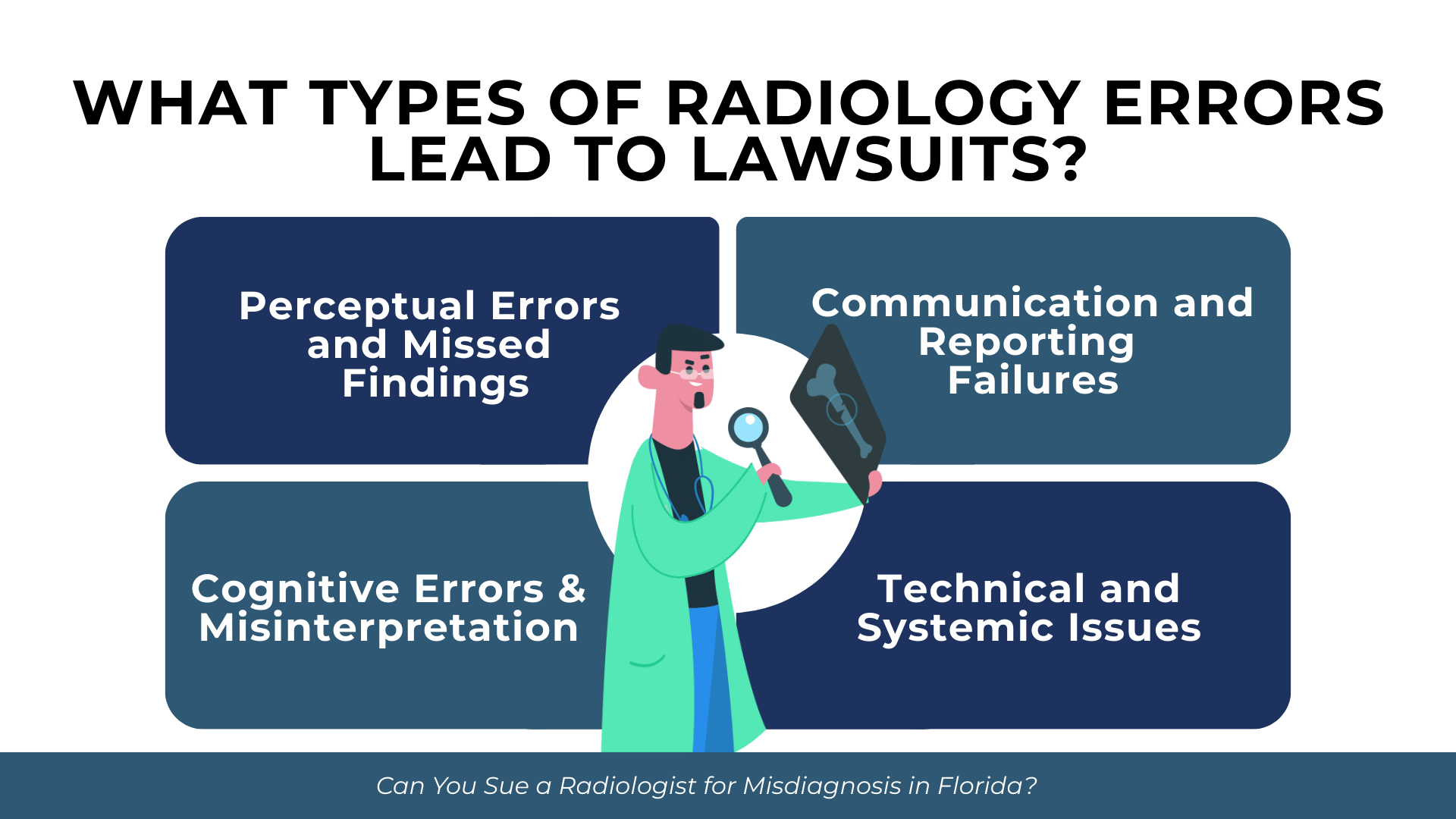
What Types of Radiology Errors Lead to Lawsuits?
Call us today at (305) 694-2676 or
contact us online for a free case evaluation.
Hablamos español.


Radiology errors fall into several categories, each with different implications for malpractice claims. Understanding these categories helps identify whether a particular error may support a legal claim.
Perceptual Errors and Missed Findings
Perceptual errors occur when a radiologist fails to detect an abnormality that is visible on the image. These represent the most common type of radiology error. A lung nodule may be present on a chest X-ray but goes unnoticed amid surrounding structures. A fracture may be visible but overlooked because the radiologist’s attention focused elsewhere.
Research identifies “satisfaction of search” as a major contributor to perceptual errors. When a radiologist identifies one abnormality, they may unconsciously stop searching for others. This cognitive pattern explains why some scans with multiple findings result in incomplete reporting.
Cognitive Errors and Misinterpretation
Cognitive errors occur when the radiologist sees a finding but interprets it incorrectly. A malignant mass may be visible and noted but characterized as benign. An early stroke may be identified but attributed to a less serious condition. These errors involve flawed clinical reasoning rather than failure to perceive.
Anchoring bias contributes to cognitive errors when radiologists fixate on an initial impression and fail to adequately consider alternatives. Prior imaging reports may create expectations that influence interpretation of current studies.
Communication and Reporting Failures
Even accurate image interpretation fails patients if findings are not communicated appropriately. A radiologist may correctly identify a suspicious lesion but fail to convey the urgency to the ordering physician. Critical findings may be documented in a report that goes unread or lacks clear recommendations for follow-up.
Communication failures can occur at multiple points: the written report itself may be unclear, verbal communication of urgent findings may not happen, or follow-up recommendations may be vague or absent. When these failures lead to delayed treatment, they may support malpractice claims.
Technical and Systemic Issues
Some radiology errors stem from factors beyond individual interpretation. Common technical and systemic issues include:
- Suboptimal image quality due to patient factors such as body habitus or inability to hold still
- Equipment malfunction or calibration issues affecting image clarity
- Inadequate clinical information provided by the ordering physician
- Excessive workload leading to rushed interpretation
- Comparison films not available or not reviewed
- Protocol errors resulting in incomplete imaging of the area of concern
- Fatigue from high-volume reading sessions
- Distractions in the reading environment
These factors may affect liability allocation when multiple parties contribute to an error. However, they do not necessarily excuse the radiologist if the error still represents a departure from acceptable practice under the circumstances.
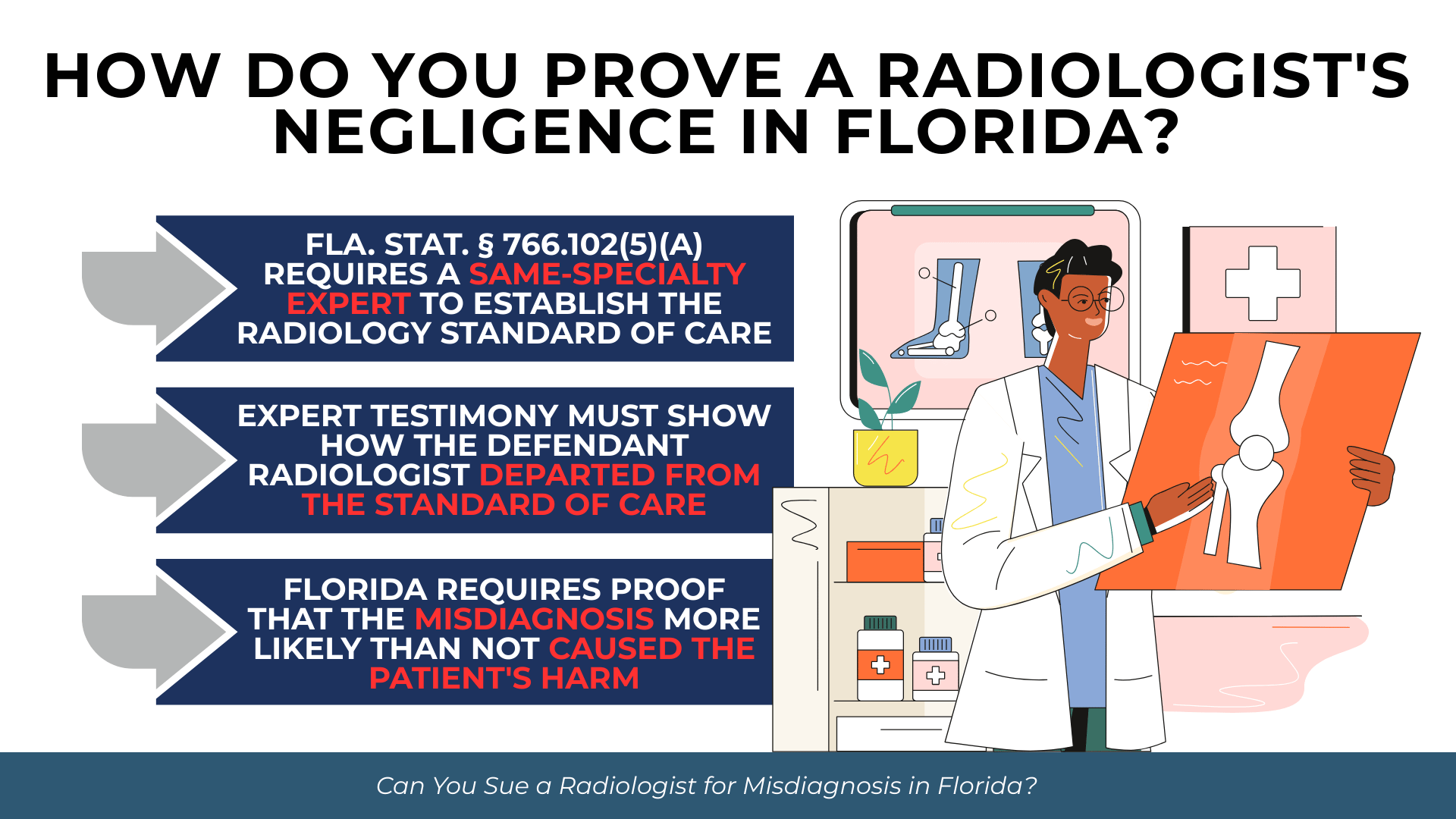
How Do You Prove a Radiologist’s Negligence in Florida?
Florida medical malpractice claims require proving four elements: (1) the applicable standard of care, (2) breach of that standard, (3) causation, and (4) damages. As established in Wale v. Barnes, 278 So. 2d 601 (Fla. 1973), these elements form the foundation of any medical negligence claim.
Establishing the Applicable Standard of Care
Because radiology is a medical specialty, Fla. Stat. § 766.102(5)(a) requires that expert witnesses specializing in the same specialty establish the standard of care. An expert testifying against a radiologist must be a radiologist who has devoted professional time during the three years immediately preceding the incident to active clinical practice, instruction, or clinical research in radiology.
The expert must review all pertinent medical records and hold an active, valid license. These requirements ensure that the standard of care is established by someone with current, relevant expertise rather than outdated or theoretical knowledge.
Demonstrating a Breach Through Expert Testimony
Expert testimony must explain how the defendant radiologist’s interpretation deviated from what reasonably prudent radiologists would do. This typically involves the expert reviewing the same images, explaining what should have been seen, and opining that the failure to identify or correctly interpret the finding fell below acceptable standards.
For certain obvious errors, res ipsa loquitur may apply. Under Marrero v. Goldsmith, 486 So. 2d 530 (Fla. 1986), this doctrine permits an inference of negligence when the injury would not ordinarily occur absent negligence and the instrumentality causing injury was under the defendant’s control. While most radiology cases require expert testimony, egregious errors may qualify for this evidentiary approach.
Proving Causation Under Florida’s “More Likely Than Not” Standard
Causation in radiology cases often presents the greatest challenge. Under Gooding v. University Hospital Building, Inc., 445 So. 2d 1015 (Fla. 1984), Florida requires proof that the misdiagnosis more likely than not caused the patient’s harm. The plaintiff must establish a greater than 50% probability that earlier diagnosis would have resulted in a better outcome.
Florida has rejected the loss of chance doctrine. If a patient’s pre-diagnosis survival rate was already below 50%, the plaintiff cannot recover even if the radiologist clearly erred. For example, if a cancer was missed but the patient’s survival odds were only 40% even with timely diagnosis, Florida law bars recovery because the misdiagnosis did not change the probable outcome.
For conditions like stroke, timing can be critical. According to AHRQ’s systematic review (2022), stroke is the leading cause of serious misdiagnosis-related harms. Missed stroke on imaging can deprive patients of time-sensitive interventions, making causation more straightforward to establish when treatment windows are missed.
What Damages Can You Recover in a Radiology Malpractice Case?
Economic Damages for Medical Costs and Lost Income
Economic damages compensate for quantifiable financial losses. In radiology malpractice cases, these typically include:
- Additional medical treatment required due to delayed diagnosis or disease progression
- Future medical expenses for ongoing care related to the worsened condition
- Lost wages during treatment and recovery periods
- Lost earning capacity if the patient can no longer work at previous levels
- Out-of-pocket costs for transportation, home modifications, or medical equipment
- Loss of household services if the patient can no longer perform domestic tasks
Florida places no cap on economic damages in medical malpractice cases. Plaintiffs may recover the full extent of their documented financial losses.
Non-Economic Damages After the Kalitan Decision
Non-economic damages address losses that lack a specific dollar value, including physical pain and suffering, mental anguish, disfigurement, loss of enjoyment of life, and loss of consortium. Following Estate of McCall v. United States, 134 So. 3d 894 (Fla. 2014) and North Broward Hospital District v. Kalitan, 219 So. 3d 49 (Fla. 2017), Florida’s statutory caps on non-economic damages in medical malpractice cases are currently unenforceable as unconstitutional under Florida’s Equal Protection Clause.
This means radiology malpractice plaintiffs can seek non-economic damages without the artificial limits that previously applied. Juries determine appropriate compensation based on the evidence presented.
When Multiple Parties May Be Liable
Radiology malpractice cases may involve multiple defendants beyond the radiologist who misread the images. Under Florida’s vicarious liability framework outlined in Fla. Stat. § 766.110, hospitals may face liability under several theories.
If the radiologist is a hospital employee, respondeat superior applies. If the radiologist is an independent contractor but the hospital held them out as staff, apparent agency under Irving v. Doctors Hospital of Lake Worth, 415 So. 2d 55 (Fla. 4th DCA 1982) may create hospital liability. The referring physician who failed to follow up on radiology findings may share responsibility. Imaging centers and their corporate owners may face direct liability for systemic failures.
Florida’s pure comparative negligence system, preserved for medical malpractice under Fla. Stat. § 768.81(6), allows recovery even if the plaintiff bears some responsibility. Damages are reduced proportionally based on fault allocation among all parties.
What Are Florida’s Pre-Suit and Procedural Requirements?
Get started with your complimentary case evaluation today;
call us at (305) 694-2676 or reach us online using our
secure contact form.


Mandatory Pre-Suit Investigation and Expert Affidavit
Florida imposes mandatory pre-suit requirements before filing a medical malpractice complaint. Under Fla. Stat. § 766.203, the claimant must complete a pre-suit investigation to determine whether reasonable grounds exist to believe the radiologist was negligent and that such negligence caused injury.
This investigation must produce a verified written medical expert opinion corroborating reasonable grounds to support the claim. The expert affidavit must come from a qualified radiologist who has reviewed the pertinent records and can attest that the claim has merit. This requirement filters out frivolous claims before litigation begins.
The Notice of Intent Process
Before filing suit, claimants must serve written Notice of Intent to initiate litigation upon each prospective defendant at least 90 days before filing. Under Fla. Stat. § 766.106(2), the notice must include:
- A list of all known healthcare providers who treated the patient for the claimed injuries
- All known providers during the two years before the alleged malpractice
- Copies of all medical records relied upon by the expert in signing the affidavit
- An executed HIPAA authorization form per Fla. Stat. § 766.1065
The 90-day pre-suit period allows defendants to investigate the claim and potentially resolve it without litigation. Defendants may respond with a rejection, settlement offer, or offer to arbitrate.
Statute of Limitations and Repose Periods
Florida’s statute of limitations for medical malpractice is two years from when the incident occurred or two years from when the incident is discovered or should have been discovered with due diligence. Under Tanner v. Hartog, 618 So. 2d 177 (Fla. 1993), discovery requires knowledge of both the injury and a reasonable possibility that it was caused by malpractice.
Radiology cases often involve delayed discovery because patients may not learn that an earlier scan was misread until a subsequent study reveals the problem. However, Florida imposes a four-year statute of repose under Fla. Stat. § 95.11(5)(c). No matter when discovery occurs, claims generally cannot be brought more than four years after the incident.
Filing a Notice of Intent tolls both the statute of limitations and the statute of repose under Musculoskeletal Inst. Chartered v. Parham, 745 So. 2d 946 (Fla. 1999). An automatic 90-day extension is available by petition to the clerk within the limitations period under Fla. Stat. § 766.104(2).
Frequently Asked Questions About Radiology Malpractice in Florida
How long do I have to file a radiology malpractice lawsuit in Florida?
You have two years from when you discovered or should have discovered both the injury and the reasonable possibility that it resulted from malpractice. However, Florida’s four-year statute of repose generally bars claims filed more than four years after the misread imaging study, regardless of when you learned about the error. Prompt legal consultation is essential to preserve your rights.
Can I sue the hospital if a radiologist missed something on my scan?
You may have a claim against the hospital depending on the radiologist’s relationship with the facility. If the radiologist was a hospital employee, the hospital faces vicarious liability. If the radiologist was an independent contractor but the hospital held them out as staff without disclosing their independent status, apparent agency may create hospital liability. The specific facts determine which theories apply.
What if the radiologist found the abnormality but failed to communicate it?
Communication failures can support malpractice claims when they result in patient harm. Even accurate interpretation fails patients if critical findings are not conveyed to the ordering physician or if the urgency is not made clear. The question is whether the radiologist’s communication met the standard of care and whether better communication would have changed the outcome.
Do I need an expert witness to sue a radiologist in Florida?
Yes. Florida law requires expert testimony to establish the standard of care and breach in medical malpractice cases involving specialists. The expert must be a radiologist who has devoted professional time during the three years before the incident to active clinical practice, instruction, or research in radiology. The expert affidavit is required before you can even file suit.
What is the most commonly missed diagnosis in radiology?
According to research cited by the American Academy of Ophthalmology/OMIC (2017), cancer represents a significant portion of missed diagnoses in imaging. The “Big Three” diagnostic failures—vascular events, infections, and cancers—account for approximately 75% of serious misdiagnosis-related harms according to research published in Diagnosis (2019). In primary care settings specifically, missed cancer represents 46% of diagnostic error malpractice claims according to the Journal of Healthcare Risk Management (2019).
Taking Action After a Radiology Misdiagnosis
Radiology errors can have profound consequences for patients and families. When a missed finding on imaging leads to delayed treatment, disease progression, or worse outcomes, Florida law provides a path to accountability and compensation. However, these cases require meeting exacting legal standards, securing qualified expert testimony, and navigating complex pre-suit requirements within strict time limits.
The intersection of medical complexity and legal procedure makes early evaluation essential. Preserving imaging studies, gathering medical records, and understanding the timeline of events all contribute to building a viable claim. The two-year discovery rule and four-year repose period mean that delay can permanently bar otherwise valid claims.
If you believe a radiologist’s error caused harm to you or a family member, contact Prosper Injury Attorneys to discuss your situation.