Stroke is a medical emergency where every minute matters. When a hospital emergency department fails to recognize stroke symptoms, the consequences can be devastating. Patients may suffer permanent brain damage, paralysis, speech impairment, or death from what could have been a treatable condition.
If you or a family member experienced a delayed or missed stroke diagnosis at a Florida hospital, you may have grounds for a medical malpractice lawsuit. However, suing a hospital involves specific legal requirements and liability theories that differ from claims against individual physicians. Understanding these distinctions is essential before pursuing legal action.
When Does Stroke Misdiagnosis Become Medical Malpractice?
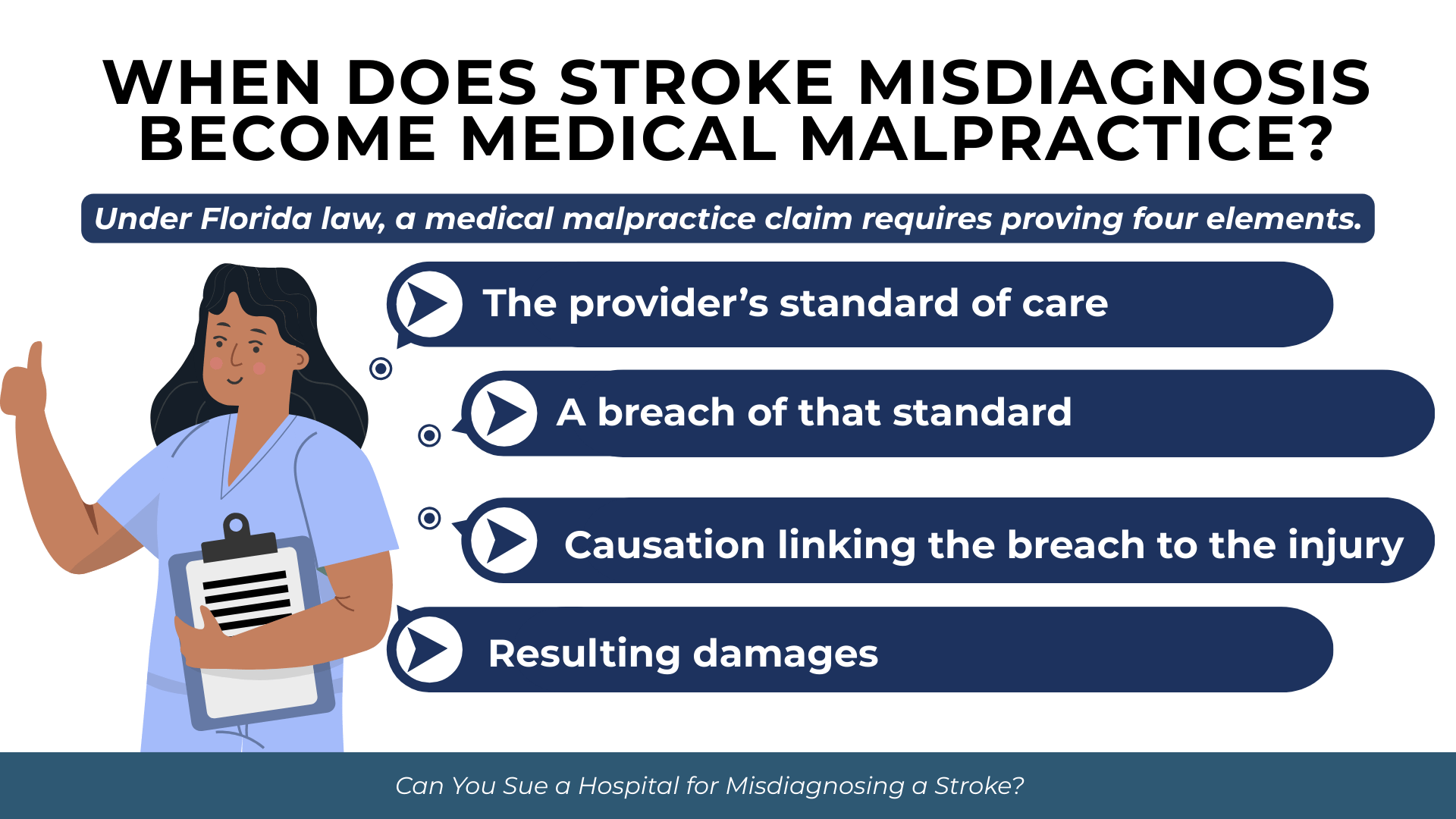
Not every diagnostic error rises to the level of medical malpractice. Florida law requires patients to prove specific elements before recovering damages for a missed or delayed diagnosis.
The Four Elements of a Florida Medical Malpractice Claim
Under Florida law, a medical malpractice claim requires proving four elements. The claimant bears the burden of establishing each by the greater weight of evidence.
These four elements are:
- The applicable standard of care that governed the healthcare provider’s conduct
- A breach of that standard through action or omission
- Proximate causation linking the breach to the patient’s injury
- Damages resulting from the negligent conduct
The prevailing professional standard of care is defined under Fla. Stat. § 766.102(1) as “that level of care, skill, and treatment which, in light of all relevant surrounding circumstances, is recognized as acceptable and appropriate by reasonably prudent similar health care providers.”
How Diagnostic Error Differs from Treatment Error
Diagnostic error cases present unique challenges compared to treatment errors. When a surgeon operates on the wrong site, the breach is often obvious. When a physician fails to diagnose a stroke, proving negligence requires demonstrating that a competent physician would have recognized the condition given the same symptoms and information.
Diagnostic failures typically involve errors in clinical judgment. A physician may have failed to order appropriate tests, misinterpreted imaging results, or dismissed symptoms that warranted further investigation. Establishing breach requires expert testimony explaining what a reasonably prudent physician should have done differently.
The Critical Role of Timing in Stroke Cases
Stroke treatment operates within narrow time windows. Tissue plasminogen activator (tPA), the primary clot-dissolving medication for ischemic stroke, must generally be administered within 4.5 hours of symptom onset. Mechanical thrombectomy may extend this window to 24 hours in certain cases.
When diagnosis is delayed beyond these treatment windows, patients may lose their only opportunity for intervention. This timing element becomes central to both breach and causation analysis. The question is not simply whether the diagnosis was eventually correct, but whether the delay fell below the standard of care and caused additional harm.
How Common Is Stroke Misdiagnosis in Emergency Departments?
Call us today at (305) 694-2676 or
contact us online for a free case evaluation.
Hablamos español.


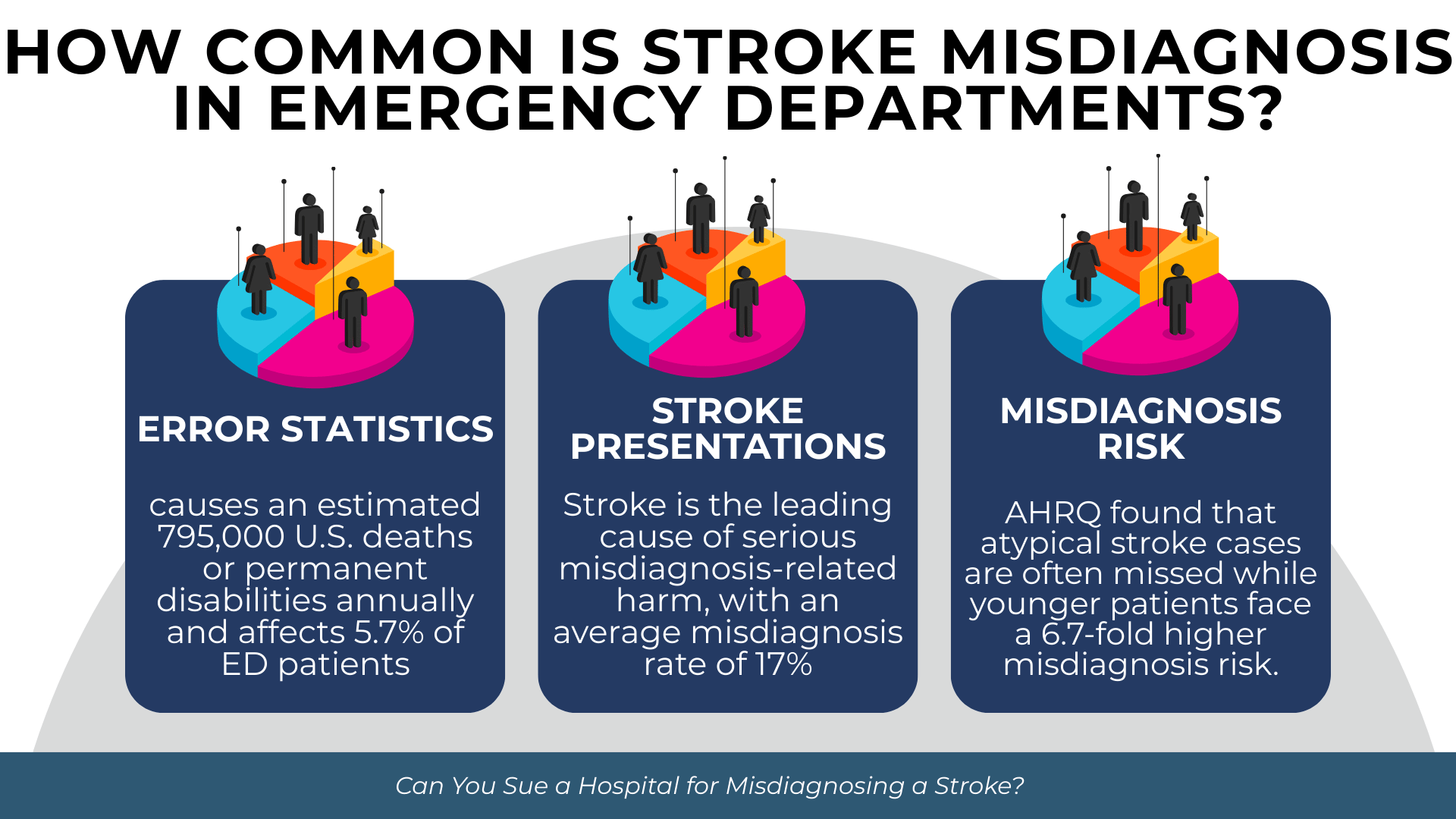
Understanding the prevalence of diagnostic error provides important context for evaluating potential claims. Research consistently demonstrates that stroke is among the most frequently missed diagnoses in emergency settings.
National Diagnostic Error Statistics
Diagnostic error represents a substantial source of preventable medical harm. According to a 2024 study published in BMJ Quality & Safety, approximately 795,000 Americans die or become permanently disabled from diagnostic error annually. This figure includes 371,000 deaths and 424,000 cases of permanent disability across all clinical settings.
Emergency departments carry particular risk. According to AHRQ’s 2022 systematic review on emergency department diagnostic errors, 5.7% of ED patients receive an incorrect diagnosis. This translates to approximately 7.4 million misdiagnoses annually across 130 million U.S. emergency department visits. The same review found that 0.3% of ED patients suffer serious harm from diagnostic error, resulting in approximately 370,000 cases of permanent disability or death each year.
Why Stroke Presentations Are Frequently Missed
Stroke ranks as the leading cause of serious misdiagnosis-related harm among all medical conditions. According to research published in BMJ Quality & Safety (2024), vascular events, infections, and cancers account for approximately 75% of all serious misdiagnosis-related harms. Stroke alone represents a substantial portion of the vascular event category.
The AHRQ systematic review found that stroke misdiagnosis rates average 17%, with a range of 9.5% to 27.3% depending on the clinical setting and patient population.
Which Symptoms Carry the Highest Misdiagnosis Risk
Not all stroke presentations face equal diagnostic challenges. Classic stroke symptoms such as facial drooping, arm weakness, and slurred speech are recognized relatively reliably. Atypical presentations create significantly greater risk.
According to AHRQ’s analysis, stroke patients presenting with dizziness or vertigo are missed approximately 40% of the time, compared to only 4% for those presenting with motor weakness symptoms. The same research found that younger age increases stroke misdiagnosis risk 6.7-fold. Physicians may not expect stroke in younger patients and attribute symptoms to more benign conditions such as migraines or inner ear problems.
How Can a Hospital Be Held Liable for a Physician’s Misdiagnosis?
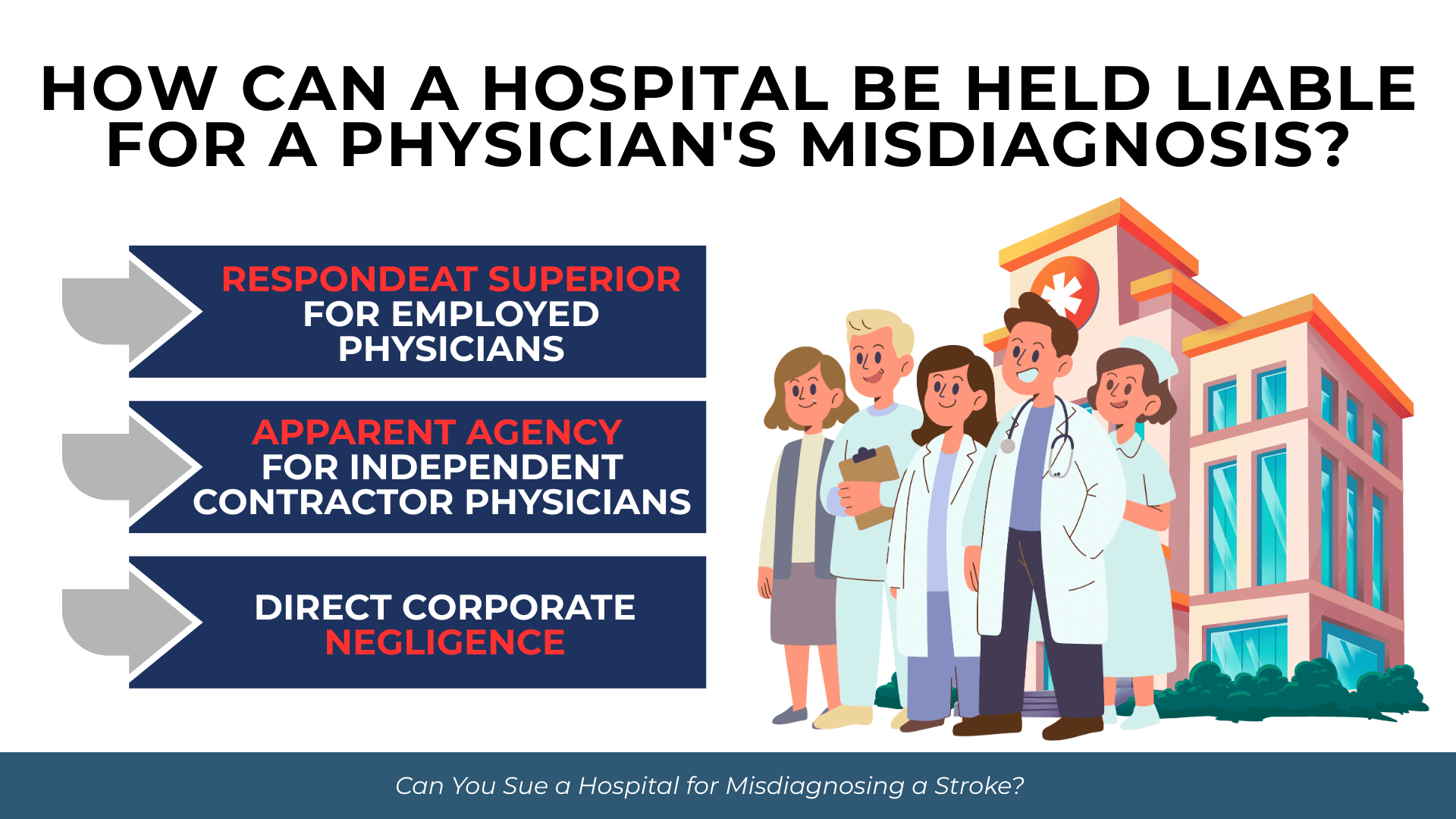
Suing a hospital rather than an individual physician requires establishing a legal basis for institutional liability. Florida recognizes several theories under which hospitals may be held responsible for physician negligence.
Respondeat Superior for Employed Physicians
When a physician is directly employed by the hospital, the hospital may be vicariously liable under respondeat superior. This Latin term means “let the master answer” and holds employers responsible for the negligent acts of employees performed within the scope of employment.
Under Fla. Stat. § 766.110, healthcare facilities have specific duties regarding staff selection, risk management, and supervision. When an employed emergency physician misdiagnoses a stroke, the hospital that employed that physician may share liability for the resulting harm.
Apparent Agency for Independent Contractor Physicians
Many emergency room physicians are independent contractors rather than hospital employees. This arrangement does not automatically shield hospitals from liability. Florida courts recognize apparent agency, also called ostensible agency, as a basis for hospital liability.
The seminal case Irving v. Doctors Hospital of Lake Worth, Inc., 415 So. 2d 55 (Fla. 4th DCA 1982), established that hospitals may be liable when they hold out a physician as their agent and the patient reasonably relies on that appearance.
Courts consider several factors when evaluating apparent agency claims:
- Hospital advertising and marketing presenting the facility as the care provider
- Uniforms, logos, and identification badges connecting staff to the hospital
- Hospital assignment of physicians to patients without patient choice
- Hospital billing practices suggesting integrated services
- Failure to disclose the physician’s independent contractor status
- The patient’s lack of opportunity to select their own provider
The three-part test articulated in Roessler v. Novak, 858 So. 2d 1158 (Fla. 2d DCA 2003), requires showing: (1) representation by the hospital, (2) reliance by the patient, and (3) a change in position based on that reliance.
Direct Corporate Negligence
Hospitals may also face direct liability for their own institutional failures. Under Fla. Stat. § 766.110, hospitals have duties regarding staff selection, credentialing, risk management programs, and supervision.
If a hospital negligently credentialed a physician with a history of diagnostic failures, or if systemic failures in emergency department protocols contributed to the misdiagnosis, the hospital itself may be directly negligent. This theory does not depend on establishing an employment or agency relationship with the misdiagnosing physician.
What Must You Prove to Sue a Hospital for Stroke Misdiagnosis?
Meeting Florida’s burden of proof in a diagnostic error case requires carefully developing evidence on each element of negligence.
Establishing the Standard of Care
The standard of care for stroke diagnosis in an emergency setting reflects what reasonably prudent emergency physicians would do under similar circumstances. Florida has largely abandoned strict locality rules in favor of a national professional standard for clinical care under Fla. Stat. § 766.102.
Expert testimony is required to establish this standard. The expert must explain what symptoms, history, and findings should have prompted the diagnosing physician to consider stroke. This typically includes discussion of recognized stroke screening protocols such as the National Institutes of Health Stroke Scale (NIHSS) and appropriate imaging studies.
Demonstrating Breach Through Expert Testimony
Under Fla. Stat. § 766.102(1), the claimant must prove that the healthcare provider’s actions represented a breach of the prevailing professional standard. This requires expert testimony identifying specific deviations from accepted practice.
In stroke misdiagnosis cases, breach may arise from failure to obtain adequate history, failure to perform appropriate neurological examination, misinterpretation of symptoms, failure to order timely imaging, or incorrect interpretation of CT or MRI results.
Meeting Florida’s Causation Standard
Causation presents perhaps the greatest challenge in diagnostic error litigation. Florida requires proof that the defendant’s negligence was the proximate cause of injury under a “more likely than not” standard exceeding 50% probability.
The landmark case Gooding v. University Hospital Building, Inc., 445 So. 2d 1015 (Fla. 1984), established this standard and rejected the loss of chance doctrine. Florida plaintiffs cannot recover for a decreased chance of survival or recovery. They must prove that, more likely than not, the patient would have had a better outcome with timely diagnosis.
The case Ruiz v. Tenet Hialeah Healthsystem, Inc., 260 So. 3d 977 (Fla. 2018), clarified that the defendant’s negligence need not be the primary cause of injury. It must only be a “substantial factor” in bringing about the harm.
In stroke cases, causation analysis focuses on whether earlier diagnosis would have permitted treatment within therapeutic windows. If a patient presented within the tPA window but was not diagnosed until after that window closed, expert testimony must establish that timely treatment would more likely than not have improved outcomes.
Documenting Damages from Delayed Diagnosis
Damages in stroke misdiagnosis cases often reflect the difference between potential outcomes with timely treatment and actual outcomes after delay. This requires careful documentation of the harm attributable to the diagnostic failure.
Common categories of harm from delayed stroke diagnosis include:
- Permanent neurological deficits that timely treatment might have prevented
- Extended hospitalization and rehabilitation needs
- Loss of independence requiring ongoing assistance
- Cognitive impairments affecting employment and daily function
- Speech and communication difficulties
- Chronic pain and reduced quality of life
Expert testimony from neurologists, rehabilitation specialists, and life care planners commonly supports damage calculations in these cases.
What Are Florida’s Pre-Suit Requirements for Diagnostic Error Claims?
Get started with your complimentary case evaluation today;
call us at (305) 694-2676 or reach us online using our
secure contact form.


Florida imposes mandatory pre-suit procedures that must be completed before filing a medical malpractice lawsuit. Failure to comply can result in dismissal.
Mandatory Pre-Suit Investigation
Under Fla. Stat. § 766.203, claimants must complete a pre-suit investigation to ascertain reasonable grounds for believing the defendant was negligent and that such negligence caused injury. This investigation must occur before serving notice of intent to sue.
The investigation typically involves obtaining complete medical records, consulting with qualified medical experts, and evaluating whether the case meets all elements of a malpractice claim.
Expert Affidavit and Notice of Intent
Before filing suit, claimants must obtain a verified written medical expert opinion corroborating reasonable grounds to support the claim. This expert affidavit must be submitted at the time the Notice of Intent is mailed.
Under Fla. Stat. § 766.106, the Notice of Intent must be served by certified mail on each prospective defendant at least 90 days before filing suit. The notice must include copies of all medical records relied upon by the expert and an executed HIPAA authorization form.
The 90-Day Screening Period
Once notice is served, a 90-day pre-suit screening period begins. During this time, defendants must investigate the claim and respond with a rejection, settlement offer, or offer to arbitrate.
Under Boyle v. Samotin, 337 So. 3d 313 (Fla. 2022), the statute of limitations is tolled from the date the Notice of Intent is mailed. The defendant’s 90-day investigation period, however, runs from the date notice is received.
What Damages Can You Recover in a Stroke Misdiagnosis Case?
Florida recognizes both economic and non-economic damages in medical malpractice cases. Understanding these categories helps evaluate the potential value of a claim.
Economic Damages
Economic damages compensate for quantifiable financial losses resulting from the misdiagnosis. These damages have no statutory cap in Florida.
Economic damages commonly include:
- Past and future medical expenses for stroke-related treatment
- Rehabilitation costs including physical, occupational, and speech therapy
- Lost wages during recovery and treatment
- Loss of future earning capacity if disability prevents return to work
- Cost of home modifications required for accessibility
- Expenses for in-home care and assistance with daily activities
Non-Economic Damages
Non-economic damages compensate for harm that cannot be easily quantified in financial terms. These include physical pain and suffering, mental anguish, loss of enjoyment of life, and disfigurement.
Florida courts permit per diem arguments that calculate non-economic damages by assigning a daily value to suffering and multiplying by expected duration.
Current Status of Damage Caps in Florida
Florida previously imposed statutory caps on non-economic damages in medical malpractice cases under Fla. Stat. § 766.118. These caps were struck down as unconstitutional.
In Estate of McCall v. United States, 134 So. 3d 894 (Fla. 2014), the Florida Supreme Court held that wrongful death non-economic damage caps violated the Equal Protection Clause. The court extended this ruling to all medical malpractice claims in North Broward Hospital District v. Kalitan, 219 So. 3d 49 (Fla. 2017).
As of December 2025, Florida has no enforceable caps on non-economic damages in medical malpractice personal injury or wrongful death cases. The statutory caps remain on the books but are not applied following these decisions.
Frequently Asked Questions About Hospital Stroke Misdiagnosis Lawsuits
How long do I have to file a stroke misdiagnosis lawsuit in Florida?
Florida’s statute of limitations for medical malpractice is two years from when the injury is discovered or should have been discovered with due diligence. Under Fla. Stat. § 95.11(5)(c), an absolute four-year statute of repose bars claims filed more than four years after the incident regardless of when discovery occurred. The case Tanner v. Hartog, 618 So. 2d 177 (Fla. 1993), established that discovery requires knowledge of both the injury and a reasonable possibility that medical malpractice caused it.
Can I sue if the emergency room doctor was not a hospital employee?
Yes. Even when emergency physicians are independent contractors, hospitals may be liable under apparent agency doctrine if the hospital held out the physician as its agent and you reasonably relied on that appearance. Factors include hospital marketing, staff uniforms and identification, billing practices, and whether you had any choice in selecting your provider.
What if I was partly responsible for the delayed diagnosis?
Florida applies pure comparative negligence to medical malpractice claims. Under Fla. Stat. § 768.81(6), the modified comparative fault rule that bars recovery when plaintiff is more than 50% at fault explicitly does not apply to medical negligence claims. Your recovery will be reduced by your percentage of fault, but you will not be barred from recovery regardless of that percentage.
Do I need a medical expert to sue for stroke misdiagnosis?
Yes. Under Fla. Stat. § 766.102, expert testimony on the standard of care is mandatory in Florida medical malpractice cases. You must also obtain a verified expert opinion before serving your Notice of Intent to sue. The expert must hold an active license and meet specific specialty-matching requirements established by statute.
What is the average settlement for stroke misdiagnosis cases?
Settlement values vary substantially based on the severity of injury, strength of liability evidence, available insurance coverage, and other case-specific factors. Florida does not publish comprehensive settlement data for diagnostic error cases. An experienced attorney can evaluate your specific circumstances after reviewing medical records and consulting with experts.
Can family members sue if the patient died from a misdiagnosed stroke?
Florida’s Wrongful Death Act allows the personal representative of the decedent’s estate to bring an action for the benefit of surviving family members. Recoverable damages vary by the relationship to the decedent and include lost support, lost companionship, and mental pain and suffering for qualifying survivors.
Conclusion
Suing a Florida hospital for stroke misdiagnosis is legally possible but requires meeting specific procedural and evidentiary requirements. You must establish that the diagnosing physician breached the standard of care, that the hospital is vicariously or directly liable for that breach, and that the delay in diagnosis more likely than not caused your injuries.
Stroke misdiagnosis claims involve substantial complexity. The factual analysis requires understanding both the medical aspects of stroke diagnosis and treatment timing, and the legal theories that connect physician negligence to hospital liability. Florida’s mandatory pre-suit requirements add additional steps that must be completed before filing.
If you believe you or a family member suffered harm from a delayed or missed stroke diagnosis at a Florida hospital, contact Prosper Injury Attorneys to discuss your situation.